
Life sciences
Precision dosing: Predicting patient-specific drug dosages
Model-informed precision dosing (MIPD) is a promising example of how doctors can use data science, and more specifically computer modelling, when predicting a patient-specific drug dosing regimen.
Executive Summary
- Background: In patients with an underactive thyroid gland (Hashimoto’s thyroiditis), it currently takes an average of 199 days to determine the correct dosage of a synthetic thyroid hormone (levothyroxine).
- Challenge: The existing dosing scheme is very generic and rarely fits the individual needs of a patient.
- Approach: Together with Radboudumc, creating a framework outlining how to develop a model from the data that can be used in practice. We then presented a proof of concept to general practitioners.
- Solutions: A dosing model that predicts a high or low levothyroxine dosage, based on an individual patient’s characteristics.
- Impact: Precision dosing has the potential to create substantial benefits for patients, general practitioners, and insurance companies.
The Background
Model-informed precision dosing is the process of optimizing dosing based on individual patient characteristics. Together with the department of General Practice at Radboud University Medical Centre (Radboudumc), we explored how both patients with Hashimoto’s thyroiditis and their physicians would benefit from precision dosing.
Hashimoto’s Thyroiditis is an autoimmune disease that causes the thyroid gland to produce too little thyroid hormone. Patients must be supplemented with a synthetic thyroid hormone (levothyroxine) to improve their symptoms. Despite levothyroxine being prescribed to half a million Dutch patients, the current dosing protocol only considers a few patient characteristics. Namely, age, weight and cardiovascular comorbidity.
Currently, it takes an average of 199 days to determine the correct dosage of levothyroxine for each patient. Precision dosing would allow for more accuracy from the outset, thus reducing the patient’s burden and cost of care.
"This study is an example of a way to use data for clinical decision-making support in general practice. You could think of hundreds of topics which, in a similar manner, could help doctors through this approach."
Prof. Henk Schers, Radboudumc
The Challenge
Typically, patients are prescribed following a standardized dosing scheme, and the clinical effect is measured from there. The challenge is that this scheme is very generic and rarely fits the individual needs of each patient. Consequently, this results in a sub-optimal clinical effect due to a lack of personalisation.
The time-frame of determining the optimal dosage is often extensive. If a patient is under-supplied, the negative symptoms associated with the disease will not improve. This often includes fatigue and constipation. Conversely, if a patient is oversupplied there can be negative side effects. These may include a rapid heart rate, headaches and mood fluctuations.
Precision dosing can address this challenge by investigating the historical treatment data. This data is already gathered through standard record-keeping in general practices. The data is analyzed to determine which dosage lead to the most optimal clinical effect in certain subgroups.
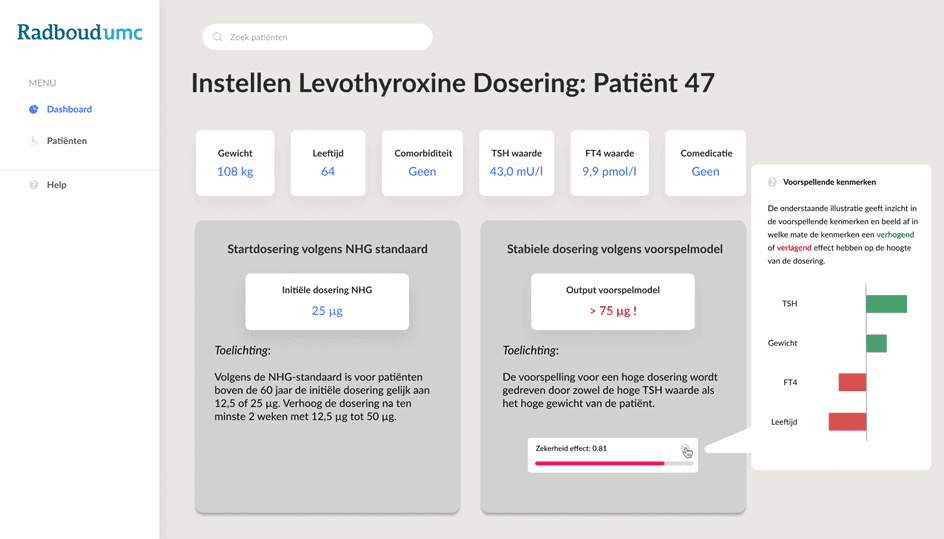
Figure 1: A visualisation of the decision support tool from the perspective of a general practitioner. At the top, the boxes outline a patient’s characteristics used to determine the dose. Below, the box on the left summarizes the current dosing scheme. The box on the right explains the dose predicted by the model, and the “zekerheld effect” is the certainty of this prediction. The pop-out box to the right visualizes the coefficients of the logistic regression model. All numbers displayed are indicative of a fictional case.
The Solutions
We started with a simple data analysis of how specific characteristics, such as age, weight, relevant hormone levels and co-medication individually contribute to the eventual dosage. The model was then developed by testing several pilot models that feature different combinations of the characteristics to see how they affect the dosage.
The selection of the final model was based on performance metrics and how easily it can be interpreted by general practitioners. This model was then fine-tuned with data scientists and doctors to minimize the risk of overdose as much as possible. In this context, an overdose, or false positive, is a prediction of a high dose for a patient who should have been prescribed a low dose.
In this framework, expanding the data set with new patient observations can increase the accuracy of the target. Currently, the model predicts in two classes that distinguish between high stable doses and low stable doses. However, we expect later models based on a more extensive data set to be able to predict in at least four dose categories.
The framework is flexible and therefore consists of a step-wise approach. It considers both the quality and quantity of the data available. The eventual aim is to develop a precision dosing model that predicts the specific stable dosage to the milligram. It will then be able to advise doctors in real-time on the correct dosage for the individual patient in the doctor’s office.
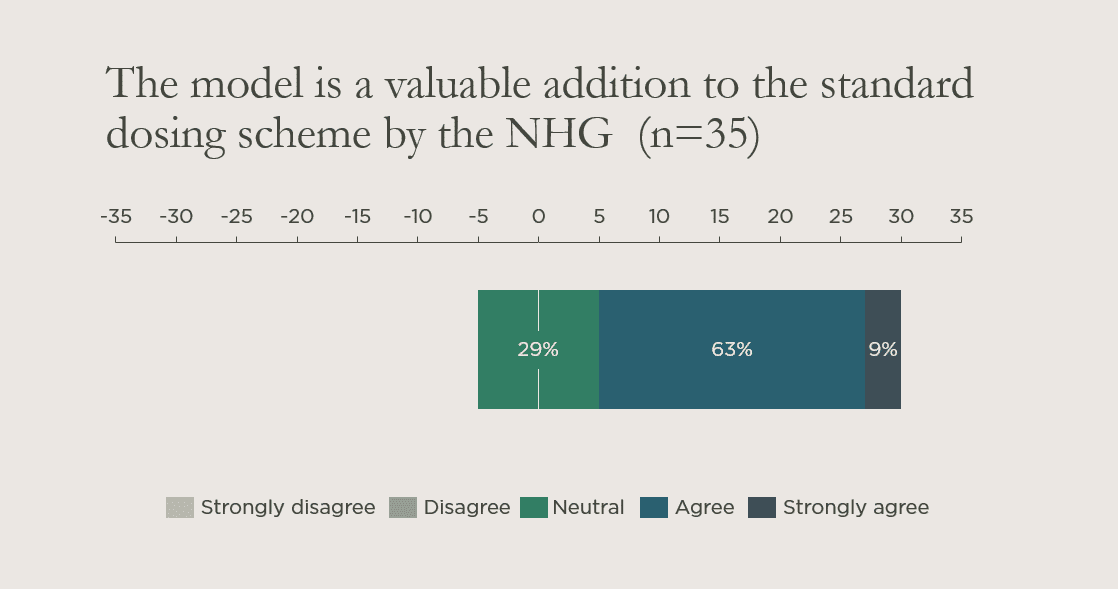
Figure 2: A visualization of one of the results from a survey conducted with 35 general practitioners in The Netherlands. The results show that all the participants either agreed with or expressed neutrality regarding the model’s added value to their practices.
The Impact
Precision dosing has the potential to create substantial impact for patients, general practitioners and insurance companies. Firstly, reducing the period to find a stable effective dosage benefits the patients. They experience symptom improvements sooner, spend less time in doctors’ offices, and get fewer lab tests done. As a result, the burden of the disease is significantly diminished.
Additionally, the feedback from general practitioners has been very positive, as seen through the results of the survey we conducted. There was a consensus that artificial intelligence (AI) can both assist them in improving their quality of care and make them more efficient.
Incorporating AI would help strengthen doctor-patient relationships. Namely, by reducing the time spent on routine, administrative tasks and creating more time for meaningful interaction. It is important to recognize that doctors still need to understand why and how a machine generates advice to feel secure in their recommendations without taking the authority of the machine for granted.
Finally, Insurance Companies, such as VGZ who funded this project, can benefit from precision dosing. The current process of determining the optimal dosage results in each patient frequently visiting his or her doctor. By reducing the average time-frame to find the optimal dosage, the cost per patient is also reduced as a result of fewer doctor visits.
Learnings for ADC
This project demonstrates how looking solely at inefficient models or business rules will at best address the symptoms. However, this will not improve the efficiency and effectiveness of the entire transaction monitoring framework. As a result, it is better to take a holistic approach where the SIRA, customer segmentation, detection methods and monitoring form a consistent framework to provide long-term improvements.

Let’s shape the future
Do you want to know more? Get in touch with Andreas Kjær (Life Science Lead).
Get in touchStay updated
Subscribe to our newsletter for insights and updates.
Connect with our experts
From shaping an AI vision to scaling solutions in production, we work with you as one team to drive AI transformation that truly brings impact.
Contact us